Shoulder Dislocations
What is a Shoulder Dislocation?
Dislocated Shoulder Symptoms And Treatment
Shoulder injuries can vary in severity, from minor strains to complete dislocations. A dislocation of any joint is when the two articulating surfaces of the joint lose complete contact with each other.
The shoulder joint is a ball and socket joint, so when the ball that is part of the upper arm bone, (aka – humeral head), moves out of range of the socket, which is part of the shoulder blade (scapula), this is known as a shoulder dislocation. Sports injuries often involve such joint dislocations due to high-impact activities.
Dislocated shoulder symptoms can vary, but often include severe pain, swelling, and an inability to move the joint.
The humeral head can move out of contact with the socket in different directions. If the humeral head moves forwards, this is known as an anterior dislocation. If the humeral head moves backwards, this is known as a posterior dislocation. If it moves downwards then this is known as an inferior dislocation.
95% of shoulder dislocations occur in the antero-inferior direction.
A subluxation (partial dislocation) is when the ball and socket move out of normal functioning range, but there is still some contact between the joint surfaces.
Complete dislocations, on the other hand, occur when the joint surfaces lose complete contact with each other.
What are the symptoms of a shoulder dislocation?
For most people, it is obvious when they dislocate their shoulder. There is usually a high-force injury that causes immediate and severe pain in the shoulder. There is loss of movement of the shoulder, and they cannot lift their arm. Dislocated shoulder symptoms may also include visible deformity and swelling. If you are not sure if your shoulder joint has dislocated, consult with a doctor.
If this is a recurrent dislocation, then there may be less pain, but most patients report that they know their shoulder is out of joint as it is difficult to move the arm.
Sometimes patients report unusual sensations running down the arm, such as tingling or pins and needles associated with shoulder injuries. Understanding the symptoms and causes of shoulder dislocations helps in determining appropriate diagnosis and treatment.
What should I do if I dislocate my shoulder?
When the shoulder joint dislocates, the shoulder muscles go into spasm and this can make it difficult to put the arm back into its correct place. If you think you have dislocated your shoulder, then seek medical attention urgently. Go to an Emergency Department for a formal assessment by a healthcare professional.
They would usually order an X-ray to confirm that it has been dislocated. Afterwards, to control the pain, you will be given some medicine either by inhaling through a mask, or through a tiny needle into your vein. Once the medicine has taken effect your arm will be manipulated and placed back into joint. You may even hear a ‘clunk’ as it goes back into place.
Another X-ray will confirm that it has been reduced back properly. Occasionally it is not possible to relocate the shoulder when you are awake due to extreme muscle spasm. In this case, you will be taken to the operating theatre and given a general anaesthetic to relax your muscles to make it easier to relocate.
Your arm will then be placed into a sling to rest it and you will be sent home and asked to attend an orthopaedic fracture clinic within a few days to be seen by a specialist.
What happens if my shoulder dislocates again?
If you have dislocated your shoulder once, with sufficient force it is more likely to dislocate again in the future. Certain risk factors for an increased possibility of another dislocation includes being male, under 20 years of age and playing contact sport such as rugby.
The older you are on your first dislocation, the less likely you are to suffer from future shoulder dislocations.
If your shoulder does happen to dislocate again, then the priority is to get it back into joint as soon as possible and this may mean going back to the Emergency Department. Shoulder instability is a common concern after recurrent dislocations.
Will I need surgery if I dislocate my shoulder?
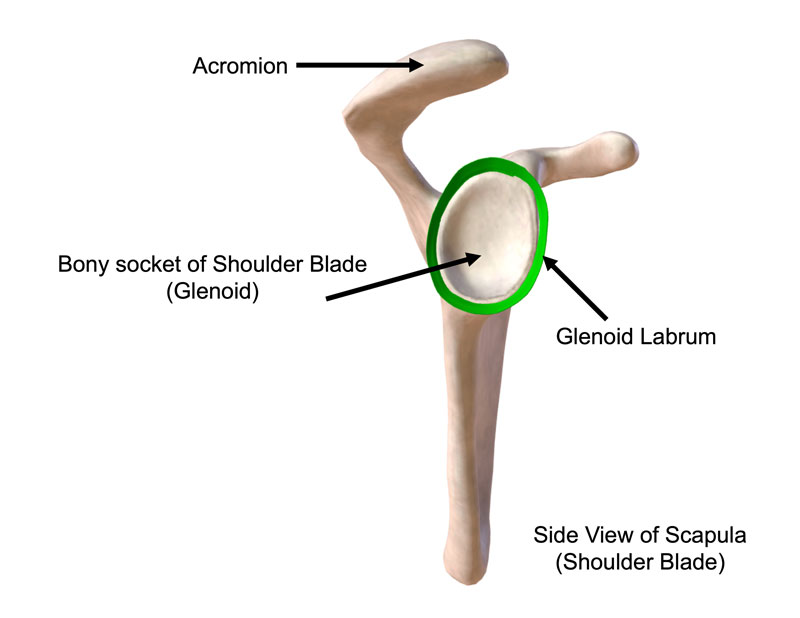
The decision to proceed with surgical treatment depends on how badly the structures within the shoulder have been torn or damaged. The shoulder is held together by a series of ligaments, muscles, and other soft tissues and any of these may be torn. There is a ring of rubbery tissue called the glenoid labrum that surrounds the bony socket (glenoid) of the scapula, which is almost always damaged in a dislocation.
Additionally, the bones may become damaged.
Most first-time shoulder dislocations do not need surgery unless there has been damage to the bones or if there are high risk factors for it occurring again (see above)
If the shoulder dislocates repeatedly then surgery will be required to repair the torn structures and stabilise the joint.
What happens during surgery to stabilise the shoulder?
Shoulder stabilisation surgery is usually a day case operation, which means you’ll typically go home at the end of the day, or if your surgery happens in the afternoon, you might have an overnight stay.
You’ll have a light general anaesthetic, and the anaesthetist will also give you a nerve block, so that you will not feel any pain in your shoulder when you wake up from surgery.
There are two ways to stabilise the shoulder. If only the soft tissues have been torn, then the repair can be done through small incisions made around the shoulder (what’s known as arthroscopic or keyhole surgery), but if there is damage to the bones, then a bigger incision will be needed to get full access to the shoulder.
In an arthroscopy, small suture anchors are placed with the bony socket and stitches are placed around the torn socket (labrum) to bring it back to the bone and secure it in place. Orthopaedic surgeons perform these procedures to stabilise the shoulder joint.
If there is bony damage to either the socket or the humeral head, then some bone will be taken from another part of the shoulder blade (coracoid process) and will be placed on the front of the socket (glenoid) and held securely in place with metal screws.
Are there any potential complications of shoulder stabilisation surgery?
Thankfully, surgery usually goes as planned. Infection or injury to structures such as blood vessels or nerves is very rare, but occasionally stiffness or some continued pain and swelling may happen after the surgery. Recurrent dislocation after surgery is around 5%. The good news is that the majority of complications can be fixed.
How long does it take to recover from
shoulder stabilisation surgery?
When you leave the hospital, your arm will be in a sling across your body to protect the surgical repair. You’ll be given some initial exercises to help prevent stiffness and physical therapy will be essential to guide you through the recovery process. Most people can gradually stop using the sling after four weeks.
Regarding return to physical activity, you can sit on a static exercise bike after a couple of days to keep your cardio fitness up as long as you keep your arm in the sling at all times. You can try gentle breaststroke swimming and jogging at around six weeks. I would advise a gradual return to specific sports. For example if you play golf, you can practise chipping at six weeks and then go to the driving range at around week eight.
Do not attempt to complete an 18-hole course at your first session. Similarly with tennis, try using a soft practice ball against a wall to regain your confidence, rather than playing a 5-set match straight away.
Post surgery FAQ
Ms Susan Alexander is a senior orthopaedic surgeon and is recognised by all the UK’s major insurers.